Contact Us
Home
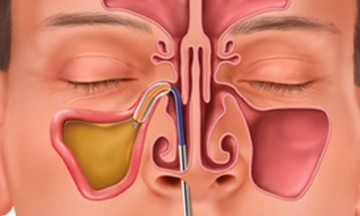
Healthcare
Sakra Premium
Clinic
Doctors
Pay
Online
Careers
Annual
Clinical Report
BMW Report
News &
Events
Nursing
Organ Transplant Organization
Symptoms